It looks like I'll be spending another weekend in the hospital. I asked the doctor this morning if I could go home today and the answer was 'no.' They want to monitor me a for a few more days on the anti-rejection medication before sending me off on my own.
My poor arms are bruised from all the IVs and blood work they have done over the last few weeks. They tried to put a PICC line in today but for some reason couldn't thread it past my shoulder. I was really rooting for them to get it as both the IVs and blood work could be done painlessly through the PICC line.
I have moved down to the 7th floor though which is both nice and irritating. It is nice because it means that I am no longer attached to the blood pressure and heart rate monitors. It is irritating because I once again have a roommate. I hope this one is quieter than my previous one. It would hard for them to be much louder.
A weekly blog that explores living post-transplant, discovering my limitations with new lungs while trying new recipes and crafting projects.
Friday 30 January 2015
Thursday 29 January 2015
No brain aneurism!
The good news is that I don't have a brain aneurism. The second CT was clear which is fantastic. I'm still feeling dizzy if I move my head too quickly though. No one seems to know why that's happening and if it's from the medication or a residual effect from the seizures. The anti-seizure medication is working though as I haven't had any more seizures.
They've started me on a new anti-rejection that hopefully has less side effects than the other one. I've also started a "lower blood pressure and heart rate" medication that seems to be working so far. A lot of these medications seem to be given as a reaction to the inital-life-saving-medication. I'm happy to take them as it means I stay alive but it seems as though I'm now trapped even more in the medication cycle.
I haven't seen the neurologist yet who I'm pretty sure gets to make the final call re: treatment of seizures. Perhaps they will grace me with their presence tomorrow so I can get out of here. As nice as the nurses are, I would rather not hang out with them all weekend if at all possible.
They've started me on a new anti-rejection that hopefully has less side effects than the other one. I've also started a "lower blood pressure and heart rate" medication that seems to be working so far. A lot of these medications seem to be given as a reaction to the inital-life-saving-medication. I'm happy to take them as it means I stay alive but it seems as though I'm now trapped even more in the medication cycle.
I haven't seen the neurologist yet who I'm pretty sure gets to make the final call re: treatment of seizures. Perhaps they will grace me with their presence tomorrow so I can get out of here. As nice as the nurses are, I would rather not hang out with them all weekend if at all possible.
Wednesday 28 January 2015
Back to the hospital...
I'm back in the hospital. Boo-erns.
Monday night (3 am), I woke up with a sharp pain in my right arm. And then my entire body went numb and passed out. It was terrifying. I woke Isaiah up with my thrashing and he called 9-11 (so I'm told, I don't remember that part), and the paramedics showed up and whisked me away to the hospital.
I had another seizure while I was on the stretcher and then two more when I was in emerg. I am now back on step-down with its constant monitoring and 2:1 nursing. At least the nurses are mostly all friendly and I already know them.
The doctors don't know what caused the seizures but their best guess is that it's a side effect from one of my anti rejection meds. The doctors started me on 'anti-seizure' pills as well as the antibiotic I had been getting over the weekend in emerg. They also started me on another med to bring down my blood pressure and heart rate. All these side-effects from the medication trying to keep my body from rejecting the lungs.
While I was out of it yesterday (I slept most of yesterday), they sent me off for a CT scan and MRI. Today I had my first EEG (that I remember anyway). If you have to choose a test to do, pick the EEG. Sure they put some jelly stuff in your hair but you get a nice scalp massage to go with it. Today, I was told that the CT scan and MRI show a possible spot or something in my brain so back I went for another CT scan, this time with dyes!
I'm pretty frustrated, I had three whole wonderful days to sleep in my own bed and eat my own food. Being back in the hospital is a total drag. Although seeing as I can barely stand up without getting a head rush, I don't think I'm going to be running out of here in a few days. I'm not sure if it's still the effects from the seizure (I know my jaw still hurts where it was clenched), or maybe it's something to do with the new meds but I hope it goes away in a few days though as it's quite unpleasant. One upside of the step-down until is that I get a room all to myself. Yay no noisy roommate!
Monday night (3 am), I woke up with a sharp pain in my right arm. And then my entire body went numb and passed out. It was terrifying. I woke Isaiah up with my thrashing and he called 9-11 (so I'm told, I don't remember that part), and the paramedics showed up and whisked me away to the hospital.
I had another seizure while I was on the stretcher and then two more when I was in emerg. I am now back on step-down with its constant monitoring and 2:1 nursing. At least the nurses are mostly all friendly and I already know them.
The doctors don't know what caused the seizures but their best guess is that it's a side effect from one of my anti rejection meds. The doctors started me on 'anti-seizure' pills as well as the antibiotic I had been getting over the weekend in emerg. They also started me on another med to bring down my blood pressure and heart rate. All these side-effects from the medication trying to keep my body from rejecting the lungs.
While I was out of it yesterday (I slept most of yesterday), they sent me off for a CT scan and MRI. Today I had my first EEG (that I remember anyway). If you have to choose a test to do, pick the EEG. Sure they put some jelly stuff in your hair but you get a nice scalp massage to go with it. Today, I was told that the CT scan and MRI show a possible spot or something in my brain so back I went for another CT scan, this time with dyes!
I'm pretty frustrated, I had three whole wonderful days to sleep in my own bed and eat my own food. Being back in the hospital is a total drag. Although seeing as I can barely stand up without getting a head rush, I don't think I'm going to be running out of here in a few days. I'm not sure if it's still the effects from the seizure (I know my jaw still hurts where it was clenched), or maybe it's something to do with the new meds but I hope it goes away in a few days though as it's quite unpleasant. One upside of the step-down until is that I get a room all to myself. Yay no noisy roommate!
Monday 26 January 2015
Home is scary
I'll be honest, it was scary on Friday to come home. Not in the 'ahhhh scary monster' way, but in the 'I don't know if I can handle being responsible for my own health' kind of way. Ive been in the hospital for so long and had people take care of all my appointments and medical decisions and responsibilities that transitioning back to doing it all myself was a bit much.
It was especially terrifying when Isaiah picked up my two giant bags of anti-rejection medication from pharmacy and it took us forever to sort though them all and figure out what was what. Even more terrifying are the needles I now have to give myself, I'm okay with needles as long as I don't have to inject the pain on myself. Although I have gotten better with the insulin needle, the blood thinner one, not so much. As least I no loner run away from thim. That much of my rational brain is working.
I think once I get into a routine it and then it will be somewhat less overwhelming.
It was especially terrifying when Isaiah picked up my two giant bags of anti-rejection medication from pharmacy and it took us forever to sort though them all and figure out what was what. Even more terrifying are the needles I now have to give myself, I'm okay with needles as long as I don't have to inject the pain on myself. Although I have gotten better with the insulin needle, the blood thinner one, not so much. As least I no loner run away from thim. That much of my rational brain is working.
I think once I get into a routine it and then it will be somewhat less overwhelming.
Sunday 25 January 2015
24 Hours
24 hours.
That's how long I made it before being summoned back to the hospital. I had a wonderful Saturday; I had a long soak in the tub (well, I couldn't really soak due to my vac dressing but my legs got a much needed soak and scrub), we opened our stockings (Merry Jan-Christmas!), organized my medication, and were just sitting down to enjoy some homemade pizza when my phone rang with a Ontario number.
I knew immediately it was the hospital and had been hoping all day that I wouldn't hear from them. The doctor confirmed that both of my Thursday and Friday blood cultures show I have an infection and that I need more antibiotics, and could I please be here 10 minutes ago. We ended up scarfing down our pizza and heading off to the emerg department. Apparently, I couldn't make it one day without having someone jab a needle into me.
The good news is that they are trying hard to not re-admit me and instead I get to use the ER as an outpatient unit. I had a dose of antibiotic last night and am returning this evening for another dose. On Monday, they will do a echocardiogram, more blood work, and I hope come up with a better plan than "visit the emerg department every night to get one IV." Although spending every evening on a stretcher in the hallway is still better than being readmitted.
That's how long I made it before being summoned back to the hospital. I had a wonderful Saturday; I had a long soak in the tub (well, I couldn't really soak due to my vac dressing but my legs got a much needed soak and scrub), we opened our stockings (Merry Jan-Christmas!), organized my medication, and were just sitting down to enjoy some homemade pizza when my phone rang with a Ontario number.
I knew immediately it was the hospital and had been hoping all day that I wouldn't hear from them. The doctor confirmed that both of my Thursday and Friday blood cultures show I have an infection and that I need more antibiotics, and could I please be here 10 minutes ago. We ended up scarfing down our pizza and heading off to the emerg department. Apparently, I couldn't make it one day without having someone jab a needle into me.
The good news is that they are trying hard to not re-admit me and instead I get to use the ER as an outpatient unit. I had a dose of antibiotic last night and am returning this evening for another dose. On Monday, they will do a echocardiogram, more blood work, and I hope come up with a better plan than "visit the emerg department every night to get one IV." Although spending every evening on a stretcher in the hallway is still better than being readmitted.
Friday 23 January 2015
Home!!!
I'm home!!! Yay!! They finally let me go around 630. The resident on call who signed me off was the same one who I had over at St. Mikes and who worked with me the night I was admitted for the transplant. It was very fitting that he was the one who officially discharged me.
I'm slightly overwhelmed to be home when I look at all the stuff I have to sort through from the past two months. Plus all the Christmas presents I haven't opened yet. I think I'll leave it all for tomorrow and do as little as possible while enjoying the silence and lack of noisy roommate.
I'm slightly overwhelmed to be home when I look at all the stuff I have to sort through from the past two months. Plus all the Christmas presents I haven't opened yet. I think I'll leave it all for tomorrow and do as little as possible while enjoying the silence and lack of noisy roommate.
Just one more thing before you go...
Discharge is a endless process. Since I was told that the plastic surgeons had decided they wouldn't operate, I was subsequently told that they might operate. In fact, they had not discharged me from their system at all, whoever told me that was vastly misinformed. Apparently the head plastic surgeon needed to look at my wound so on Wed poked around the area and confirmed it was healing nicely with the vac machine. He did say that they might have to do a skin graft to finish the closing of the wound but that wouldn't be for several weeks.
Since I was cleared by plastics to be discharged, I met with the post-transplant admin assistant who set up all my post-transplant information. She is who I contact anytime I have problems or need an appointment. I have all my stuff prepped for next week as well as info on the microspirometer that I need to buy.
Yesterday, I really thought I was going home, homecare was arranged (the social work finally got the paperwork figured out), meds were ordered from pharmacy, and goodbyes had been said by all. Then I felt nauseous, started vomiting, and my heartrate spiked while walking to physio. I felt nauseous for most of the day so the doctors didn't feel comfortable discharging me and ha bloodwork drawn. I was super frustrated but it's hard to argue while curled up in bed around a basin.
Today looks like it might be the real deal. The doctors are concerned about infection as one of my cultures from yesterday shows that something is growing but it's too early to know what. The doctor said it may be a false positive so my blood work was retaken. I'm told they'll call me if they have horrible news for me to return to hospital. Its still worth fleeing for a night, even if I have to return.
I am pretty much all set to go, I have my discharge papers from pharmacy, I was switched over to the mini vac machine that I'll be using at home, and Isaiah has carted stuff off to the car. I was actually given the "pack up!" by my nurse at one point only to have her come in and say "just one more dose of IV antibiotics before you go." Of course that involved putting in a new IV which meant 2 nurses and 5 more pokes before they could get one in my tiny tortured veins.
We are now just waiting for the IV to finish running before we break out of here. I'm trying to force myself not to get excited until I've actually left the ward and they can no longer haul me back for more testing.
Since I was cleared by plastics to be discharged, I met with the post-transplant admin assistant who set up all my post-transplant information. She is who I contact anytime I have problems or need an appointment. I have all my stuff prepped for next week as well as info on the microspirometer that I need to buy.
Yesterday, I really thought I was going home, homecare was arranged (the social work finally got the paperwork figured out), meds were ordered from pharmacy, and goodbyes had been said by all. Then I felt nauseous, started vomiting, and my heartrate spiked while walking to physio. I felt nauseous for most of the day so the doctors didn't feel comfortable discharging me and ha bloodwork drawn. I was super frustrated but it's hard to argue while curled up in bed around a basin.
Today looks like it might be the real deal. The doctors are concerned about infection as one of my cultures from yesterday shows that something is growing but it's too early to know what. The doctor said it may be a false positive so my blood work was retaken. I'm told they'll call me if they have horrible news for me to return to hospital. Its still worth fleeing for a night, even if I have to return.
I am pretty much all set to go, I have my discharge papers from pharmacy, I was switched over to the mini vac machine that I'll be using at home, and Isaiah has carted stuff off to the car. I was actually given the "pack up!" by my nurse at one point only to have her come in and say "just one more dose of IV antibiotics before you go." Of course that involved putting in a new IV which meant 2 nurses and 5 more pokes before they could get one in my tiny tortured veins.
We are now just waiting for the IV to finish running before we break out of here. I'm trying to force myself not to get excited until I've actually left the ward and they can no longer haul me back for more testing.
Monday 19 January 2015
No surgery from plastics.
Update: no extra surgery from plastics for me, hurray!
But that is all I know. I don't know why they decided not to operate, or what that means about the wound healing. The nurse had a one minute phone conversation with them that they weren't operating and that I was off their caseload. So I also don't know when this means I can go home although I'm assuming (for the second time) by the end of the week as waiting for plastics seemed to be the only thing keeping me here.
Last week, I had been told that the social worker had all the paperwork ready re:funding for home care and the vac machine. Today I was told that the attending doctor had stopped the process by writing orders that I was going home with a regular dressing instead of the vac - which is crazy because everyone who looks at my wound says the vac machine is the best healing option. So now the paperwork needs to be refilled which is clearly going to take more phone calls and more time with me spent waiting here instead of being at home. The social worker nor the nurses nor I are very happy with this doctor.
The lung transplant team was going to come by at 530 to review everything and write the official discharge note. They have not yet shown up. I suspect they will be here bright and early AM when I'm still waking up and have forgotten all my questions. My questions such as: "when can I go home?, " "why did the stupid doctor delay the paperwork process?," and "can I leave now?"
So yay, discharge this week for real this time?!? I'm trying so hard not to get too excited but OMG I just want out of here.
But that is all I know. I don't know why they decided not to operate, or what that means about the wound healing. The nurse had a one minute phone conversation with them that they weren't operating and that I was off their caseload. So I also don't know when this means I can go home although I'm assuming (for the second time) by the end of the week as waiting for plastics seemed to be the only thing keeping me here.
Last week, I had been told that the social worker had all the paperwork ready re:funding for home care and the vac machine. Today I was told that the attending doctor had stopped the process by writing orders that I was going home with a regular dressing instead of the vac - which is crazy because everyone who looks at my wound says the vac machine is the best healing option. So now the paperwork needs to be refilled which is clearly going to take more phone calls and more time with me spent waiting here instead of being at home. The social worker nor the nurses nor I are very happy with this doctor.
The lung transplant team was going to come by at 530 to review everything and write the official discharge note. They have not yet shown up. I suspect they will be here bright and early AM when I'm still waking up and have forgotten all my questions. My questions such as: "when can I go home?, " "why did the stupid doctor delay the paperwork process?," and "can I leave now?"
So yay, discharge this week for real this time?!? I'm trying so hard not to get too excited but OMG I just want out of here.
Sunday 18 January 2015
Photos: Adventure to Sick Kids
I finally got my quiet weekend. The only real news from the doctors is that my white blood count levels are low and remain low and they aren't quite sure why. They are still working on the balance between having my medication levels high enough to avoid rejection but low enough that it doesn't completely destroy what little immune system remains. They will monitor the problem through continual blood work checks.
We decided this lazy Sunday was as good of a time as any to try to find the mysterious tunnel linking TGH to the Sick Kids hospital and the Princess Margaret hospital. I thought it would be fun to see what the food court at Sick Kids offered by way of food-variety. Turns out, not very much.
Here is our photo blog of the creepy basement walk:
We decided this lazy Sunday was as good of a time as any to try to find the mysterious tunnel linking TGH to the Sick Kids hospital and the Princess Margaret hospital. I thought it would be fun to see what the food court at Sick Kids offered by way of food-variety. Turns out, not very much.
Here is our photo blog of the creepy basement walk:
 |
| To the basement we go! Kind of looks like a horror movie starts. |
 |
| Please don't let there be a murderer in these hallways... |
 |
| There was a strange noise coming from this room. |
 |
| We found the hallway where hospital beds, computers, and desks go to die despite the one persons signage effort. |
 |
| Someone killed the Easter Bunny!! |
 |
| Maybe it was the asbestos. |
 |
| We emerged from the basement to find a fun library. We knew we were in the right place. |
 |
| Found it! Sick Kids is so much cooler than the adults. All hospitals should have libraries and giant bear statues. |
Saturday 17 January 2015
Still waiting.
*crickets chirping*
That is all I've heard from the plastic surgeons yesterday. And the lung team won't move forward with anything until they hear from plastics.
So here I sit and wait. Me and my vac machine.
That is all I've heard from the plastic surgeons yesterday. And the lung team won't move forward with anything until they hear from plastics.
So here I sit and wait. Me and my vac machine.
Thursday 15 January 2015
A update in limbo
Just a quick update to say that there is no real update re: returning back to surgery for the wound. I went for a CT scan yesterday only to be told today that the doctor had ordered the wrong kind. Or, according to the doctor, they ordered the right kind but the techs didn't do it...?
Either way, wires were crossed and I was sent back down today for another CT scan, this time involving being injected with the crazy-make-you-feel-like-you're-peeing-dye. I really hope this was the right one so they can figure out an action plan. I'm still on the floor's discharge board with the 16th in question marks but I'm no longer hopeful that it will actually happen tomorrow.
Positive updates: I'm back to a regular diet again (yay!) and things are going well in the treadmill room. I may have a wound that no one can agree on how to heal but at least I can munch on some chips while they figure it out.
Either way, wires were crossed and I was sent back down today for another CT scan, this time involving being injected with the crazy-make-you-feel-like-you're-peeing-dye. I really hope this was the right one so they can figure out an action plan. I'm still on the floor's discharge board with the 16th in question marks but I'm no longer hopeful that it will actually happen tomorrow.
Positive updates: I'm back to a regular diet again (yay!) and things are going well in the treadmill room. I may have a wound that no one can agree on how to heal but at least I can munch on some chips while they figure it out.
Wednesday 14 January 2015
Mid week update
I have decided that this hospital thrives on bringing my hopes up only to crush them beneath it's cold uniform walls.
On Sunday, things were looking all set for discharge by the end of this week. The social worker, along with the CF nurse from Halifax, figured out all the funding for the vac machine and home care. Everything was finalized yesterday with direct billing and everything only for me to be told that my wound needs more surgery.
Yes. Another surgery for me.
The lung and surgerical team decided this week to call in the plastic surgeons for consult and aid in closing my wound. Yesterday, one of the plastic surgeons told me that without them operating the wound isn't going to heal well on its own, even with the wonder of the vac machine. He also said that operating would speed up the process by months.
I don't want another surgery. I want to go home. I was told I was going home this week and I was in complete 'going home mode.' I don't want to go back to the cold OR. Or have more IVs, or another cathedar. Or waking up being completely confused and thirsty. Or more time spent in this place with its lack of privacy and 1-ply toliet paper. I want my own bed dammit.
I know, I know, "these things happen" and "it's just another bump" and "it's better to do it now than have to come back" and "it is what it is." I keep telling myself all of those things but for some reason none of them are super comforting.
The idea of another operation scares me. My body has gone through so much that to need another one so soon is overwhelming. And it's not the actual procedure itself that is freaking me out. It's the anatestic and having to be vented again. The whole 'put under' step is most dangerous part of most surgeries and my body is already so weak. I'm also terrified this will lead to furthur complications which will lead to further complications which will.....you get the idea.
All of this may not even happen of course, the plastic surgeons want a recent CT scan before they'll commit to anything. Plus, they have to figure out where they are going to get the extra muscle to cover up the wound. The actual procedure involves taking muscle from somewhere else (yet to be determined), move things around, slap on a skin graft from bum tissue, put on a pressure vac for a week, and voila! one healed wound.
So now I'm stuck here waiting for tests instead of packing to go home. The vac machine is still happily sucking up goo from the wound. Stupid wound.
Sunday 11 January 2015
7th floor pictures
I'm having a lazy Sunday so I think it's a good day for more pictures.
 |
| "My" walker. |
 |
| Slightly lighter than pushing one of these beasts around. |
 |
| The unit floor likes to be encouraging as well all do laps. |
 |
| My little shot of morning medication. |
 |
| More card making! Of the non-Christmas variety this time. |
Saturday 10 January 2015
Discharge planning
I only have one line left. Yay! My PICC line came out yesterday and my little wound drainage line was out the day before.
My last line is the vac machine which I don't anticipate losing soon. The good news is that I can go home with it. And there is talk about going home by mid-to-end of next week, yay! Discharge planning has begun!
Yesterday I, along with 4 older men, did medication training with the pharmacists. It was basically a review of all the anti-rejection medications that we will be taking for the rest of our lives. The pharmacist spent an hour scaring us about all the horrible side effects the meds can cause. She also went over the signs of infection and rejection. We were all given a goodie bag of our own medication and sent on our way. I'm now responsible for self-medicating myself (for my anti-rejection meds, with the strict supervision of a nurse) for the next few days.
The discharge coordinator, who I met a few days ago, also stopped by to review everything I need to happen before I'm discharged. She also reviewed all the ways to look for infection and signs of rejection. Everyone loves talking about watching for infection and rejection. This is going to turn me into do hypochondriac.
I can see the light toward the way out of here. Yay!!! I realized yesterday that I've been in the hospital for two months, including my pre-transplant stint at St. Mikes. I can't believe it's been six weeks since my surgery.
I'm ready to go home.
My last line is the vac machine which I don't anticipate losing soon. The good news is that I can go home with it. And there is talk about going home by mid-to-end of next week, yay! Discharge planning has begun!
Yesterday I, along with 4 older men, did medication training with the pharmacists. It was basically a review of all the anti-rejection medications that we will be taking for the rest of our lives. The pharmacist spent an hour scaring us about all the horrible side effects the meds can cause. She also went over the signs of infection and rejection. We were all given a goodie bag of our own medication and sent on our way. I'm now responsible for self-medicating myself (for my anti-rejection meds, with the strict supervision of a nurse) for the next few days.
The discharge coordinator, who I met a few days ago, also stopped by to review everything I need to happen before I'm discharged. She also reviewed all the ways to look for infection and signs of rejection. Everyone loves talking about watching for infection and rejection. This is going to turn me into do hypochondriac.
I can see the light toward the way out of here. Yay!!! I realized yesterday that I've been in the hospital for two months, including my pre-transplant stint at St. Mikes. I can't believe it's been six weeks since my surgery.
I'm ready to go home.
Thursday 8 January 2015
Back to treadmill room!
I started back in the treadmill room today! The floor physiotherapist decided that I was ready to start up again to which I was more than willingly to agree. Sometimes it's nice when the hospital is giant and all the programs are under the same roof.
I'm ready to get some of my muscles back. I was so excited to get my green card (reminder: yellow-pretransplant, green-posttransplant), it was actually a little scary how happy it made me. Even with everything I've been through, somehow holding the green card made the fact that I made it/am making it through transplant so much more real.
They don't want me to do anything in the upper area yet due to the wound so I walked slowly on the treadmill for 20 min and did some leg weights (a whole 3lb!). It felt so good to be back exercising. I walked for 20 min and my stats didn't drop below 95%. And I may have coughed three times.
At the time it didn't feel like I did much but writing this out, I now appreciate how different it is from before. It's like I've already taken for granted the fact that I don't cough every time I exert myself slightly or feel fatigued or sit around. The exercise wasn't strenuous in any way but it was enough to make me feel as though I'll sleep well tonight.
I totally understand why everyone else post-transplant was annoyingly chipper and all they talked about was how good they felt. Because it feels so good to be able to walk for 20 min and not get short of breath. You just want to tell everyone else to "work as hard as possible now!" and "don't give up!" Or I would if I were the type of person who started conversations with other people. I'll just send them the message telepathically.
I'm ready to get some of my muscles back. I was so excited to get my green card (reminder: yellow-pretransplant, green-posttransplant), it was actually a little scary how happy it made me. Even with everything I've been through, somehow holding the green card made the fact that I made it/am making it through transplant so much more real.
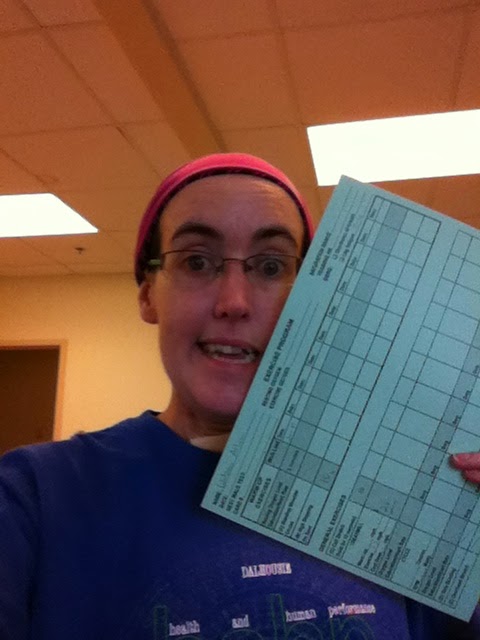 |
| Yay green sheet! |
At the time it didn't feel like I did much but writing this out, I now appreciate how different it is from before. It's like I've already taken for granted the fact that I don't cough every time I exert myself slightly or feel fatigued or sit around. The exercise wasn't strenuous in any way but it was enough to make me feel as though I'll sleep well tonight.
I totally understand why everyone else post-transplant was annoyingly chipper and all they talked about was how good they felt. Because it feels so good to be able to walk for 20 min and not get short of breath. You just want to tell everyone else to "work as hard as possible now!" and "don't give up!" Or I would if I were the type of person who started conversations with other people. I'll just send them the message telepathically.
Wednesday 7 January 2015
Goodbye elephant nose!
The NG (feeding tube) is out! Yay! I'm now officially responsible for all my own caloric and pill intake. Eek!
The strangest part was after it came out, my first thought was "I can't breathe" and then "wait a second...that makes no sense." It's as though the pressure in my nose was tricking my brain somehow to thinking I was still wearing nasal prongs.
And I don't even mean tricking my brain, I just mean that the feeling of having something in my nose has become so associated with oxygen and breathing easier that apparently even an NG tube was doing the trick. Once I convinced my lungs that they did not, in fact, need help from a feeding tube in order to get air, it felt so good to have the tube out. One less line to worry about.
I have my face back! My poor tape-sticky-residue-face.
With the pill swallowing, I'm swallowing my tiny pills and then the rest are being broken up into applesauce (I'm eating a lot of applesauce these days). Today was my first day with this system and so far the small capsules are making it down no problem. Soon enough I'll be ready for the four Creon I reflexively put in my mouth before supper tonight. I was at the point of starting to take a drink before I realized what I was doing and stopped. Oh habits, how you are trying to choke me.
As for the food, I'm still on a soft diet for swallowing but that basically means anything but stringy, raw, seedy, or crunchy food. The swallowing is going much better. There is a lot of food available in that open window that I have been throughly enjoying. In traditional hospital style, I have amassed a pile of snacky or meal-type replacement foods in my room.
I've heard unpleasant things about the food here but I honestly feel they haven't been that bad (although I couldn't eat anything 10 days ago so who am I to judge). I mean they are very hit and miss but for mass produced food, they give it a solid effort. I've had fresh fruit, hot tea, and at least the mashed potatoes don't arrive with a weird crusty top on them. *cough* *cough* Halifax *cough*
Tuesday 6 January 2015
Lungs
It's been a quiet few days. I've managed to sleep off most of the medication and effects from 'the night of the blood.' A few quiet days are fine with me. My excitement seems to all happen at once and intensely so I need time to recover in between. There have been a few progressions; I got the clearance to walk without my walker if I can find a friend to lug my vac machine for me; I may start exercising back in the physio room again; and I'm no longer on night feeds so the NG tube will be coming out soon!
I'm sure you've noticed that most of my posts have been about all the secondary 'incidents,' we'll call them, and not about my actual lungs.
My lungs? My lungs are amazing. Apart from some minor fluid on the sides, the fact that I still can't cough yet, and that I never breathe deep enough, things are currently smooth sailing.
Why haven't I written a post about how fabulous they feel yet? Partly because I'm still in shock and also because I'm blocking off that emotional waterfall until I have more energy to process it. Right now I feel like my focus is on hospital/get better mode. I'm doing what I need to in order to get out of here and it's taking all my energy.
That said, I still can't believe I'm on room air and able to breathe comfortably. It seems as though there was such a fast transition between using 1L oxygen for walking and stating low 90% to being on room air and stating at 95-96%. It's so unfathomable to me that I keep stopping at the various monitors to check my oxygen levels when walking around the unit.
The other reason I'm not raving about how amazing it is to be able to breathe is that for the first time in a long time, I don't need to think about it. I don't start coughing every time I walk anywhere or get slightly winded and it's becoming effortless. It's astounding how easy the body adjusts to change, for better or worse. And this is so very much overwhelmingly better that I can't wrap my mind around it just yet.
I'm sure you've noticed that most of my posts have been about all the secondary 'incidents,' we'll call them, and not about my actual lungs.
My lungs? My lungs are amazing. Apart from some minor fluid on the sides, the fact that I still can't cough yet, and that I never breathe deep enough, things are currently smooth sailing.
Why haven't I written a post about how fabulous they feel yet? Partly because I'm still in shock and also because I'm blocking off that emotional waterfall until I have more energy to process it. Right now I feel like my focus is on hospital/get better mode. I'm doing what I need to in order to get out of here and it's taking all my energy.
That said, I still can't believe I'm on room air and able to breathe comfortably. It seems as though there was such a fast transition between using 1L oxygen for walking and stating low 90% to being on room air and stating at 95-96%. It's so unfathomable to me that I keep stopping at the various monitors to check my oxygen levels when walking around the unit.
The other reason I'm not raving about how amazing it is to be able to breathe is that for the first time in a long time, I don't need to think about it. I don't start coughing every time I walk anywhere or get slightly winded and it's becoming effortless. It's astounding how easy the body adjusts to change, for better or worse. And this is so very much overwhelmingly better that I can't wrap my mind around it just yet.
7th floor snowtree!
Sunday 4 January 2015
Please sir, may I please have one more unit of blood?
I had a post started last night about how I hope I didn't give people the wrong impression that things weren't going well. They are moving steadily upward. I was all set to ramble on about why I was/am so frustrated about this infection when everything else is moving along swimmingly.
But then I thought it would be more fun to tell you about last night adventures. For some reason my 'quiet weekends' end up not being so quiet.
During the day, my vac dressing was finally changed (it didn't get done on Friday due to 'orders' not being in) which was much less painful than the previous time. All was well and quiet until midnight when I noticed that there was some bloody leaking happening from my site at one side. I told the night nurse who reinforced the spot with another bandage. I assumed it was because the day nurses went a little overboard with the saline rinse and weren't super careful about getting it all out.
Woke up 20 min later for it to have soaked through that as well as my gown.
On and off for the next hour or so she tried to contain the leak by adding progressively different and more types of tapes and gauzes. On and off went underpads and gowns. She declared victory at one point and I was able to sleep for awhile.
I was woken to the sound of a loud beeping a few hours later, glanced down at my chest, only to realize I had been shot.
Or, you know, the vac dressing had started leaking through yet another gown but this time ine a perfect circle on my chest.
The nurse, by then, had already arrived on the scene due to the high pitch screech coming from the machine. [Sidenote: somehow my roommate slept through all of this, the entire night. I'm not sure what medication they give her but I heard her say this morning "I had the best sleep ever!"]
The nurse decided she, along with a back up nurse, would have to change the entire dressing. However, once they started removing the dressing, they realized the bleeding was out of their control and called in reinforcement. Reinforcement (head nurse), took off the upper taping and decided to call in the resident. The resident glaced at it and the amount of blood I had lost and decided to call the surgeon. And the blood bank.
That is exactly what I wanted to hear last night, that the surgeon was being called due to the giant wound in my chest. At that point I started to think this was more than just using too much saline.
In the meantime of all this referring me to people, other nurses were running around like mad, emptying my room of any unnecessary furniture (there was none), taking massive amounts of bloodwork, cleaning up the blood that was all over me and the bed, and then retaking more blood work when they thought of something else that should be tested.
Then I was told that the surgeon decided to come in to see what was happening and make a formal assessment. That is when the worst case scenarios began to play out in my mind. Would I go back to OR? Would I need a skin graft? Do I have a wound full of blood (no one would remove the black foam to see what was happening underneath)? How long will this new thing set me back for?
My night nurse reassured me by saying that it's not unusual for people to have to go back to the OR for a second 'washing' of the wound. Thanks nurse.
I must have dozed off a little as I woke to the surgeon arriving and it was all hands on deck. He had no qualms about poking into the black foam and then subsequently taking it out. I was not filled with blood but there was bleeding happening. The chaos resumed with people rushing in and out of my room getting various equipment. It was all a bit much.
Part of the reason of why everything seemed so chaotic is because I'm in such a small place. Picture a hospital bed, and then a upright chair, a sink, and place them side-by-side, and thats about the amount of space in my room. When you have more than one person in my room at a time it seems cramped. Add in a surgeon, resident, head nurse, night nurse, and float nurse, and I started to feel slightly overwhelmed.
So they gave me some Ativan.
The surgeon continued to poke around the wound to find the cause of all the blood. It was not uber pleasant so the head nurse declared that I needed more pain medication (no complaints from me) and I was swiftly connected to another IV and had some Dilaudad (even stronger pain meds) pushed through my system.
Thankfully, the source of the bleed was just an irritated blood vessel that stopped bleeding once some pressure was applied (and not, as the surgeon kept saying, a busted artery as apparently they are exposed). I did not have to go back to the OR for a second wash and there was no need for anything else to happen. The surgeon put regular gauze in the site and decided it would all be reassessed in the morning.
Everyone cleared out, a unit of blood arrived from the blood bank to replenish all that I had lost, and I started drifting off into a very stoned sleep. But then I woke up because I kept thinking people were in my room to do more stuff in my wound. I would open my eyes and clearly no one was there but the second I closed them, I was positive that people were in my room. I was very much out of it.
At one point I pressed the call bell for no reason I can explain other than I wanted to tell someone about the people in my room. A nurse came in and I told him I was seeing people when I closed my eyes and he asked "do you see them now?" I responded indignantly "of course not, my eyes are open, they're only there when I close my eyes."
He slowly backed out of the room...
I eventually passed out for a few hours. I woke up when a nurse came in to change my feeds and they noticed that there was once again blood everywhere. This time it was way darker and way less terrifying looking. I would have panicked except I was still half knocked out. Turns out this bloody mess was due to someone, no one would admit responsibility, not reconnecting me to the blood unit and it had bled all over my bed. The charge nurse was not pleased.
I did eventually get the unit of blood and the vac dressing was reconnected in the afternoon once it was determined that the entire episode was caused by the one little blood vessel.
But then I thought it would be more fun to tell you about last night adventures. For some reason my 'quiet weekends' end up not being so quiet.
During the day, my vac dressing was finally changed (it didn't get done on Friday due to 'orders' not being in) which was much less painful than the previous time. All was well and quiet until midnight when I noticed that there was some bloody leaking happening from my site at one side. I told the night nurse who reinforced the spot with another bandage. I assumed it was because the day nurses went a little overboard with the saline rinse and weren't super careful about getting it all out.
Woke up 20 min later for it to have soaked through that as well as my gown.
On and off for the next hour or so she tried to contain the leak by adding progressively different and more types of tapes and gauzes. On and off went underpads and gowns. She declared victory at one point and I was able to sleep for awhile.
I was woken to the sound of a loud beeping a few hours later, glanced down at my chest, only to realize I had been shot.
Or, you know, the vac dressing had started leaking through yet another gown but this time ine a perfect circle on my chest.
The nurse, by then, had already arrived on the scene due to the high pitch screech coming from the machine. [Sidenote: somehow my roommate slept through all of this, the entire night. I'm not sure what medication they give her but I heard her say this morning "I had the best sleep ever!"]
The nurse decided she, along with a back up nurse, would have to change the entire dressing. However, once they started removing the dressing, they realized the bleeding was out of their control and called in reinforcement. Reinforcement (head nurse), took off the upper taping and decided to call in the resident. The resident glaced at it and the amount of blood I had lost and decided to call the surgeon. And the blood bank.
That is exactly what I wanted to hear last night, that the surgeon was being called due to the giant wound in my chest. At that point I started to think this was more than just using too much saline.
In the meantime of all this referring me to people, other nurses were running around like mad, emptying my room of any unnecessary furniture (there was none), taking massive amounts of bloodwork, cleaning up the blood that was all over me and the bed, and then retaking more blood work when they thought of something else that should be tested.
Then I was told that the surgeon decided to come in to see what was happening and make a formal assessment. That is when the worst case scenarios began to play out in my mind. Would I go back to OR? Would I need a skin graft? Do I have a wound full of blood (no one would remove the black foam to see what was happening underneath)? How long will this new thing set me back for?
My night nurse reassured me by saying that it's not unusual for people to have to go back to the OR for a second 'washing' of the wound. Thanks nurse.
I must have dozed off a little as I woke to the surgeon arriving and it was all hands on deck. He had no qualms about poking into the black foam and then subsequently taking it out. I was not filled with blood but there was bleeding happening. The chaos resumed with people rushing in and out of my room getting various equipment. It was all a bit much.
Part of the reason of why everything seemed so chaotic is because I'm in such a small place. Picture a hospital bed, and then a upright chair, a sink, and place them side-by-side, and thats about the amount of space in my room. When you have more than one person in my room at a time it seems cramped. Add in a surgeon, resident, head nurse, night nurse, and float nurse, and I started to feel slightly overwhelmed.
So they gave me some Ativan.
The surgeon continued to poke around the wound to find the cause of all the blood. It was not uber pleasant so the head nurse declared that I needed more pain medication (no complaints from me) and I was swiftly connected to another IV and had some Dilaudad (even stronger pain meds) pushed through my system.
Thankfully, the source of the bleed was just an irritated blood vessel that stopped bleeding once some pressure was applied (and not, as the surgeon kept saying, a busted artery as apparently they are exposed). I did not have to go back to the OR for a second wash and there was no need for anything else to happen. The surgeon put regular gauze in the site and decided it would all be reassessed in the morning.
Everyone cleared out, a unit of blood arrived from the blood bank to replenish all that I had lost, and I started drifting off into a very stoned sleep. But then I woke up because I kept thinking people were in my room to do more stuff in my wound. I would open my eyes and clearly no one was there but the second I closed them, I was positive that people were in my room. I was very much out of it.
At one point I pressed the call bell for no reason I can explain other than I wanted to tell someone about the people in my room. A nurse came in and I told him I was seeing people when I closed my eyes and he asked "do you see them now?" I responded indignantly "of course not, my eyes are open, they're only there when I close my eyes."
He slowly backed out of the room...
I eventually passed out for a few hours. I woke up when a nurse came in to change my feeds and they noticed that there was once again blood everywhere. This time it was way darker and way less terrifying looking. I would have panicked except I was still half knocked out. Turns out this bloody mess was due to someone, no one would admit responsibility, not reconnecting me to the blood unit and it had bled all over my bed. The charge nurse was not pleased.
I did eventually get the unit of blood and the vac dressing was reconnected in the afternoon once it was determined that the entire episode was caused by the one little blood vessel.
Saturday 3 January 2015
Some loose ends
I mentioned in passing that the 7th floor is quite different than the other floors. The nursing ratio is 4:1 compared to the 2:1 in step-down. Those ratios are the official ratios until someone goes on break and then it always seems to be there is never anyone around. So basically, less hands-on care. No more nurse-on-call (I have to get my own ice chips!). It's like a real hospital experience with a roommate and all.
I thought I would review some things that I've mentioned but have never really followed up on:
Food: Ever since the trach has come out, swallowing has gotten easier. My throat is still very raw (especially since the 29th OR visit) and the muscles aren't all there yet but it's improving slowly. It goes way better when I don't overthink it. I still have my NG tube (or elephant nose as I call it) and am getting feeds during the night to supplement my diet until I'm back to eating regularly. Providing my appetite holds steady, the dietitian and I are hoping the tube can be removed early next week.
I can not express enough how amazing everything tastes. My taste buds have never been happier. I sent Isaiah for a frapp on New Years Eve and it was magical. The food court's greasy Chinese yesterday was delightful. And even the cafeteria's mashed potatoes weren't half bad. This magical rediscovering foods must be what makes everyone forget how horrible it was to go without.
Walking: Physio has been quite hands off ever since moving to step-down and especially on 7th. They walked with me a few times and then gave me the green light to walk around with family. They also moved me from the standing to the regular walker which is clearly way easier to maueuver (the standing walkers here are beasts).
Since then, they've checked in a few times to see how I'm doing but haven't taken me out to do anything. I think with the holidays they been low staff. I'm okay with being left to my own devices. Isaiah and I have been walking around every day and just having to do everything myself is quite exhausting.
GI: Everything seems to be holding up nicely. I think I've actually been officially discharged from their system. No news is good news.
Blood clot: I assume it's still there...no one had told me otherwise. They have not done another CT to check it out so it must be ok on all my X-rays. Or at least not growing. They've done multiple ultrasounds on my legs to see if I have more and I actually think they are planning on another one. That was about a week ago and no one has rushed in with a ultrasound machine so clearly it's not their top concern.
Lungs: I guess I should talk about my lungs themselves, they are doing well! They've dried out thanks to the broncs and Lasix. I still can't quite cough yet but I'm working on it. The painful sternum doesn't help so it's good there isn't that much to cough up. I'm on roomair! I went yesterday without oxygen and walked without it fine. Last night the nurse checked my stats a few times and I held steady at 95%. Woohoo!!
Anything else I've forgotten, feel free to ask away!
I can not express enough how amazing everything tastes. My taste buds have never been happier. I sent Isaiah for a frapp on New Years Eve and it was magical. The food court's greasy Chinese yesterday was delightful. And even the cafeteria's mashed potatoes weren't half bad. This magical rediscovering foods must be what makes everyone forget how horrible it was to go without.
Walking: Physio has been quite hands off ever since moving to step-down and especially on 7th. They walked with me a few times and then gave me the green light to walk around with family. They also moved me from the standing to the regular walker which is clearly way easier to maueuver (the standing walkers here are beasts).
Since then, they've checked in a few times to see how I'm doing but haven't taken me out to do anything. I think with the holidays they been low staff. I'm okay with being left to my own devices. Isaiah and I have been walking around every day and just having to do everything myself is quite exhausting.
GI: Everything seems to be holding up nicely. I think I've actually been officially discharged from their system. No news is good news.
Blood clot: I assume it's still there...no one had told me otherwise. They have not done another CT to check it out so it must be ok on all my X-rays. Or at least not growing. They've done multiple ultrasounds on my legs to see if I have more and I actually think they are planning on another one. That was about a week ago and no one has rushed in with a ultrasound machine so clearly it's not their top concern.
Lungs: I guess I should talk about my lungs themselves, they are doing well! They've dried out thanks to the broncs and Lasix. I still can't quite cough yet but I'm working on it. The painful sternum doesn't help so it's good there isn't that much to cough up. I'm on roomair! I went yesterday without oxygen and walked without it fine. Last night the nurse checked my stats a few times and I held steady at 95%. Woohoo!!
Anything else I've forgotten, feel free to ask away!
Thursday 1 January 2015
Vac Pac Machine
While I'm super frustrated at my giant incision wound, I'm also super fascinated by what they are doing to heal it.
The incision started oozing very slowly and all the nurses attributed it to the Lasix and general drainage. In fact, when I told one of the nurses it turned into an infection, she looked personally offended. As though it could never be infected because otherwise she would have caught it. I don't think anyone would have caught it as there were zero indicators until it was too late. Thankfully, all the cultures have so far come back negative for a bacterial infection so they think it may have been a fungal thing.
How the vacuum dressing works, or at least for me (or from what I've been able to gleen from this process), is that they start by placing a small barrier pad on any exposed bones (for me, that is a small bit of the sternum), pack the wound with black foam (not the white kind as it sticks more, very important!), and tape it up with whatever the medical equivalent of packing tape over everything to make sure no air gets out. Add a suction device to the tape and attach that to a machine and voila! One vac-pac dressing done.
The machine is on continuous suction mode which means that I constantly have the small pressure and tiny vibrations going through me. I tend to notice it more at night or when I'm laying down. It's like mini-chest physio. Or like being on a boat when you feel the rumbling of the engines at first but after awhile you stop noticing.
The dressing itself is changed two or three times a week. The wound care nurse told me it would be painful (I'll be
honest, the most painful part was the tape coming off) and to press my
happy button a few times ahead of time but she didn't prepare me for the
weirdness of it all. It's one thing to be in physical pain, it's another thing to have people poking at what you know is your insides while you try to go to your happy place. Although having the doctor poke at the exposed bone and ask 'does this hurt', was not super pleasant.
As the wound gets smaller, and the amount of black foam I watch them pack into my wound shrinks (it seemed like a lot of foam), I'm sure it will be easier. Having it done three times a week will also get me use to the process. I will most likely go home with this dressing and machine and either followed up by home care or come into the hospital for the change. I shudder at the thought of all that tape being ripped off my skin. Someone needs to invent tape that only sticks when necessary and then a button is pushed and it falls off. I feel as though we have the technology for this, why hasn't it happened yet!?
The incision started oozing very slowly and all the nurses attributed it to the Lasix and general drainage. In fact, when I told one of the nurses it turned into an infection, she looked personally offended. As though it could never be infected because otherwise she would have caught it. I don't think anyone would have caught it as there were zero indicators until it was too late. Thankfully, all the cultures have so far come back negative for a bacterial infection so they think it may have been a fungal thing.
How the vacuum dressing works, or at least for me (or from what I've been able to gleen from this process), is that they start by placing a small barrier pad on any exposed bones (for me, that is a small bit of the sternum), pack the wound with black foam (not the white kind as it sticks more, very important!), and tape it up with whatever the medical equivalent of packing tape over everything to make sure no air gets out. Add a suction device to the tape and attach that to a machine and voila! One vac-pac dressing done.
 |
| The machine to which I'm now perma-attached. |
 |
| Watching the blood-goo go through the line. It's a great way to pass the time. |
As the wound gets smaller, and the amount of black foam I watch them pack into my wound shrinks (it seemed like a lot of foam), I'm sure it will be easier. Having it done three times a week will also get me use to the process. I will most likely go home with this dressing and machine and either followed up by home care or come into the hospital for the change. I shudder at the thought of all that tape being ripped off my skin. Someone needs to invent tape that only sticks when necessary and then a button is pushed and it falls off. I feel as though we have the technology for this, why hasn't it happened yet!?
Subscribe to:
Posts (Atom)

